Have you ever wondered why some days pass comfortably while others begin with burning discomfort that disrupts your focus before you even start your morning routine? Many people describe this contrast as unpredictable, but hemorrhoids usually follow a clear pattern shaped by diet, daily movement and long sitting periods. According to our editor’s research, most individuals wait too long before seeking guidance because symptoms appear mild at first and seem manageable. This delay often allows the swollen veins to progress and create persistent discomfort. When conservative treatments fail, family doctors and specialists usually consider surgical approaches that offer longer lasting relief. Understanding these procedures helps reduce fear, clarify expectations and support more confident decision making.
Why do hemorrhoids sometimes require surgery?
Hemorrhoids often respond to lifestyle changes and simple treatments, yet some cases progress despite careful attention. Doctors evaluate severity based on bleeding patterns, swelling and prolapse frequency. As a result of our editor’s reviews, many patients reach the surgical stage because symptoms interfere with work routines or everyday comfort. Surgery becomes appropriate when hemorrhoids repeatedly slip outside the anal opening or cause persistent irritation that does not improve with topical care. Identifying this threshold early prevents worsening inflammation. Understanding why surgery becomes necessary helps people feel more prepared for the next steps.
How does your doctor evaluate surgical need?
Doctors begin by assessing the type and grade of hemorrhoids you experience. Internal hemorrhoids behave differently from external ones because their pain patterns vary. According to our editor’s research, specialist evaluation focuses on bleeding volume, protrusion degree and impact on daily comfort. Some cases require imaging or further examination to rule out additional issues. Doctors consider your overall health, recovery expectations and daily habits before recommending surgery. This approach ensures that the chosen treatment aligns with your personal needs. Open communication helps you understand each detail before deciding.
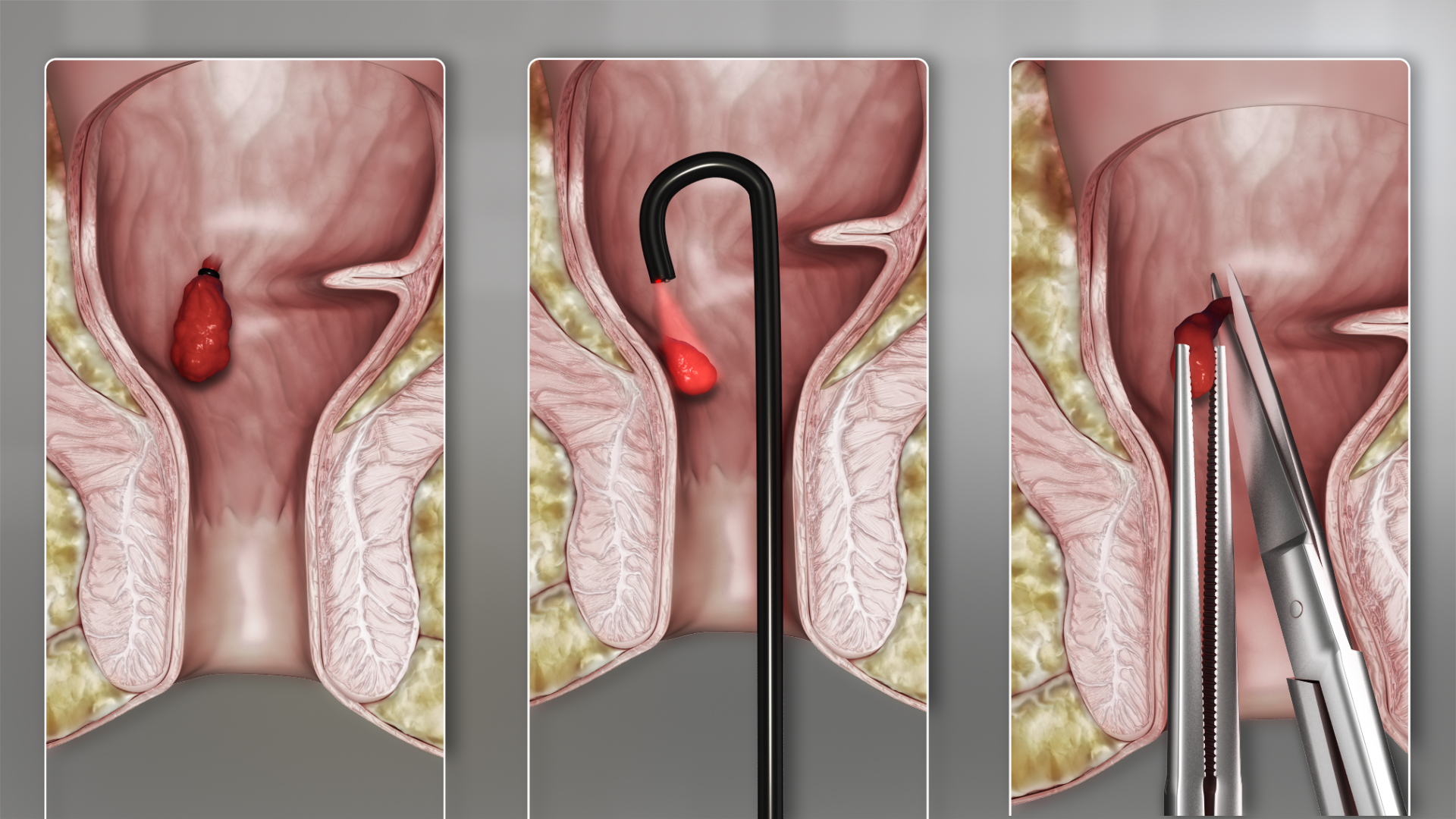
What is rubber band ligation?
Rubber band ligation remains one of the most common and straightforward surgical techniques for treating internal hemorrhoids. The procedure places a small band at the base of the swollen vein. This band restricts blood flow and allows the hemorrhoid to shrink naturally. As a result of our editor’s reviews, many patients appreciate this method because it offers quick recovery and minimal discomfort. Doctors usually recommend it for moderate internal hemorrhoids that protrude intermittently. The band typically falls off within a week during normal bowel movements. Knowing how this technique works helps reduce anxiety before treatment.
How effective is sclerotherapy?
Sclerotherapy involves injecting a special solution directly into the hemorrhoid to shrink the tissue. Doctors use this treatment for smaller internal hemorrhoids that bleed frequently. According to our editor’s research, sclerotherapy provides relief when patients prefer a fast and minimally invasive option. The procedure takes a short time and requires no significant recovery. The injected solution causes controlled inflammation that reduces vein size. This option works best when hemorrhoids are small but persistent. Understanding its benefits helps you choose the right approach with your doctor’s guidance.
What happens during infrared coagulation?
Infrared coagulation uses focused light energy to heat and shrink hemorrhoid tissue. Specialists apply a controlled burst of infrared light to seal the vein. As a result of our editor’s reviews, many patients find this option appealing because it creates limited discomfort and allows quick return to daily routines. Doctors often choose this method when bleeding is the primary symptom. The heat reduces blood flow and supports tissue healing without significant downtime. Learning how this method works helps you feel more confident about your treatment path.
Why is hemorrhoidectomy sometimes necessary?
Hemorrhoidectomy becomes necessary when hemorrhoids reach advanced stages or cause severe pain. The procedure removes swollen tissue completely through precise surgical techniques. According to our editor’s research, doctors usually recommend hemorrhoidectomy when other treatments fail or when hemorrhoids prolapse permanently. Although recovery may take longer compared to less invasive methods, hemorrhoidectomy offers strong long term results. Many patients experience significant relief once healing progresses. Understanding the reasons behind choosing this method reduces stress before surgery and clarifies expectations.
How does stapled hemorrhoidopexy work?
Stapled hemorrhoidopexy treats internal hemorrhoids by repositioning the swollen tissue back inside the rectum. The procedure uses a circular stapling device to reduce blood flow and stabilize the hemorrhoid. As a result of our editor’s reviews, many specialists prefer this technique for patients seeking less postoperative pain than traditional hemorrhoidectomy. The stapler reshapes tissue rather than removing it completely. This method works best for prolapsing internal hemorrhoids. Knowing the advantages of stapled techniques helps patients evaluate their options with clarity.
How do doctors minimize discomfort after surgery?
Doctors provide clear aftercare plans to support recovery following hemorrhoid procedures. Pain relief medications help reduce inflammation and allow comfortable movement. According to our editor’s research, warm sitz baths improve circulation and ease swelling. Fiber rich meals support smooth bowel movements and reduce strain on healing tissue. Hydration also plays an important role because it softens stool naturally. Specialists encourage light activity to promote blood flow without stressing the surgical area. Following these guidelines creates a smoother recovery process and reduces postoperative concerns.
What should you expect during recovery?
Recovery varies depending on the chosen surgical method and individual healing patterns. Some procedures allow return to daily routines within days, while others require more patience. As a result of our editor’s reviews, patients who follow postoperative instructions closely experience faster comfort. Mild bleeding or tenderness may appear during early healing stages. These symptoms usually improve steadily without complications. Doctors monitor progress through follow up visits to ensure proper healing. Understanding typical recovery patterns reduces anxiety and helps you stay attentive to your body’s needs.
Why follow up visits matter?
Follow up appointments play a critical role in ensuring the surgical area heals correctly and without complications. Doctors assess tissue recovery and provide additional guidance when necessary. According to our editor’s research, consistent follow up reduces the risk of recurrence. Specialists may adjust dietary recommendations or suggest supportive treatments during these visits. Keeping these appointments strengthens long term results and helps maintain comfort. Paying attention to follow up care protects your recovery and prevents unnecessary strain.
How lifestyle habits support long term relief?
Surgery provides significant relief, but daily habits shape your long term comfort. A fiber rich diet reduces pressure by supporting smooth bowel movements. Adequate hydration softens stool and prevents strain. As a result of our editor’s reviews, patients who adopt consistent habits feel less discomfort over time. Regular movement improves circulation and prevents excessive sitting pressure. Good toilet practices such as avoiding long sitting periods also protect the surgical area. These small habits help maintain results and support healthier routines.
What role does mental comfort play in recovery?
Emotional comfort influences how you experience recovery and adapt to new habits. Many patients feel anxious before and after procedures because hemorrhoid symptoms affect daily confidence. According to our editor’s research, reassurance from doctors helps reduce worry and promotes steadier healing. Understanding your treatment plan encourages active participation in recovery. Emotional readiness supports physical healing by reducing stress related tension. Recognizing this connection helps you approach the process with calm and clarity.